FEBRUARY 2020
Greetings to all of our Victorian Infant Collaborative Study Families. Welcome to the 2019/2020 edition of our newsletter
Firstly a big thankyou to all of our 2016/2017 Cohort families who came along with some very busy 2 year olds.
We have almost completed the 2 year phase of the study, with RWH completely finished, Mercy and Monash should be completed very soon.
If there are any RWH participant families who were not able to attend this year, but would still like to, please don’t hesitate to contact Marion.
It is really wonderful to see how some of our smallest and sickest babies are now thriving, active toddlers.
We have some families that have become firm friends, sharing many similar experiences in their time in the neonatal unit. so very important for parents to have each other for support/ friendship and lovely friendships for the children.

This is a photo of a great catch up
when one of the families flew down from Brisbane to attend a 2 year follow up. Their faces say it all.

Eli and his mum Erin, returned to the Women’s for his 2 year VICS assessment.
One of our pin up babies for the Royal Women’s Hospital.
This is the window
at the Grattan Street entrance of the hospital. Lovely to see how much Eli has
grown in 2 years.
Vics 2005 Update
2020 study on physical activity habits in the VICS 2005 cohort

The Murdoch Children’s Research Institute, at the Royal Children’s Hospital is conducting a new study, commencing February / March 2020. A biomedical science honor’s student by the name of Molly Muir will be conducting this. The aim of the study is to assess the physical activity and exercise habits of adolescents born extremely pre-term, in comparison to those born at full gestation. It will be looking to see if there are any differences in patterns and attitudes to exercise between these groups, through the use of five survey questionnaires. Whilst the focus is on determining if there are any disparities between groups, we will also be using data from a separate study that measures a variety of heart and respiratory parameters, to see if there are correlations to habit and attitudes to exercise, and the underlying physiological differences in those born extremely pre-term. The surveys will be distributed via email, and it would be greatly appreciated if those contacted could spare the required 20-25 minutes to fill out and submit the surveys upon completion. For your interest, all results will be made available to you, later in the year.
Molly will be contacting our VICS 2005 cohort very soon.
If you have any changes to contact details please let our hospital coordinators know.
CARDIAC CYCLE STUDY

An Exciting new opportunity for some of our Royal Women’s Hospital 2005 VICS Cohort
The aim of the Cardiac Cycle study is to provide an understanding of how extremely preterm birth/extremely low birth weight is related to cardiopulmonary responses to submaximal and maximal exercise conditions, and to a ten-week training intervention in adolescents. A key aspect of what we do is focusing on the incorporation of technology to help participants have an engaging and motivating experience. Participants will be given a stationary bike trainer, heart rate monitor, and speed sensor, as well as an activity tracker. Participants will set up the trainer in their home and undergo a ten-week training program starting at light-moderate intensity and progressing to vigorous-moderate intensity. To help motivate participants and create a seamless avenue for remote monitoring, participants will use the virtual-reality cycling app Zwift and the fitness tracking app Strava. Zwift allows cyclists to virtually ride on roads/tracks all over the world (e.g. New York, London, mountains, islands, even around volcanos), with the virtual bike/rider controlled via the Bluetooth-enabled speed sensor attached to the physical bike. Heart rate is displayed on the monitor and can be used to attain/maintain the target value. After each session, data will upload automatically onto Strava, which has built-in features designed to break through common barriers to exercise. The research coordinator can track the participant’s rides, alerting us to waning motivation and enabling positive reinforcement. Our approach of making the exercise intervention feel more like a game than a task is an innovative method that may have broad impact beyond this project.
Marion has been and will be continuing to contact eligible participants. Please let her know if you are interested (Royal Women’s Hospital births only)
1991-1992 Cohort
This is Emily Oliver and her baby daughter Lara.
Emily is one of our VICS 191/1992 birth cohort participants. Emily was a very tiny baby, born at 26 weeks, with a birthweight of a mere 910 grams. She has a twin brother Tom.
Emily had a great day with us when she returned for assessment at 25 years old. Thank-you Emily. Emily is now mum to a pre term baby of her own. Lara was born at 32 weeks, weighing in at 2.1kg.


Emily asked us a very interesting question-
I am curious to know if there is a link between myself being a prem and then having a prem child? I know there are many other factors that can cause this.
This is a question many of you (especially young women of child bearing age) may be thinking.
As far as our research has proven, this is the answer so far-
It has been documented that women who were born preterm themselves, have a higher prevalence of preterm offspring. This is from studies in the Netherlands and Scandinavia. We have yet to document that in the Australian population, as VICS is the largest study and the follow up for the 91-92 cohort is only 25 years. The older VICS cohorts did not report of reproductive outcomes.
Thank you for sharing some of your story with us Emily.
High blood pressure in young adults born preterm
We completed health assessments (physical and mental) for our Victorian Infant Collaborative Study (VICS) young adult study (91-92 cohort) in 2018. Our next important step was to collate and examine the results from various health assessments and report the outcomes to the wider community. Early this year, we presented some of the results from this study at the Perinatal Society of Australia and New Zealand conference.
Publications from the 25 year old follow up of the 1991-92 cohort –
High blood pressure in young adults born preterm
Babies born very tiny or very small are surviving into adulthood in increasing numbers. It is therefore important to understand the long term health outcomes. In the VICS 91-92 cohort we measured blood pressure at 25 years of age. We showed that young adults born very tiny or very early were at increased risk of high blood pressure as compared to those born normal birthweight.
Given that blood pressure can be managed if detected in a timely manner, it is important for the health community, families and individuals themselves to be aware of the risk of high blood pressure in those born very early and very little.
Haikerwal A, Doyle LW, Cheung MM, Wark JD, Opie G, Roberts G, Patton G, Cheong JLY. Hypertension. 2020 Jan;75(1):211-217

Peter and Leigh visiting our nursery wearing their 24 hour BP monitors. Thankyou.
Some interesting information pertinent to lung health that has been reported from our cohorts.
Airway obstruction in young adults born extremely preterm or extremely low birth weight in the post surfactant era
Doyle LW, Irving L, Haikerwal A, Lee K, Ranganathan S, Cheong J.
Thorax 2019; 74:1147-1153

The ability to get air in and out of the lungs increases through childhood, reaches a peak in the early 20s, and then gradually declines with increasing age. Children who are born extremely early (before 28 weeks of pregnancy) of extremely low birthweight (<1000 g), have more problems as a group with airflow in and out of their lungs. Those preterm and tiny children who developed a condition called bronchopulmonary dysplasia in the newborn period have even more trouble with airflow. However, it is unclear if children born extremely early or tiny are reaching their full airway growth potential into their early 20s. In this study we compared airflow at 25 years and from 8 to 25 years of participants born <28 weeks or <1000 g with controls who had been born of normal birthweight, and within the preterm group we compared those who had bronchopulmonary dysplasia with those who did not. Just over one-half of all the children born in Victoria in 1991 or 1992 who survived and a similar proportion of the controls had breathing tests at 25 years of age; more had had breathing tests at either 8 years or 18 years of age.
Airflow was substantially reduced in the preterm group compared with controls, and even more so in those preterm participants who had bronchopulmonary dysplasia in the newborn period. Airflow growth was less between 8 and 18 years of age for the preterm group compared with controls, but not between 18 and 25 years.
Overall the results mean that the preterm participants, as a group, are not reaching their full airway potential by their early 20s. Approximately 25% of the preterm group had airflow low enough to be concerning for their future health, but this means that 75% had normal airflow. It will be important to assess both groups again as they age to establish if their rate of decline in airflow is normal or if it is excessive.
Since smoking will accelerate the rate of decline in airflow, it should be avoided as much as possible. If anyone is worried about their breathing they should consult their doctor.
MARK TRAYLING
At Monash Children’s hospital we regularly have past premature children visiting us to say hello or to check in at important moments in their lives, such as gradation, or turning 18 or 21 years of age, to remind themselves and their parents of how grateful they are to be alive.
We recently had a visit from one of our past premature cohort who was born in 1981, at our previous hospital, known then as the Queen Victoria hospital. Mark was born at just 25 weeks gestation and weighed 820gms.
Mark remembered being a participant in our long-term follow up program and coming many times for ‘check-ups’. Looking at the hospital archives he was assessed at the ages of 1, 2, 5, 8 and 14 years.
Mark was keen to visit the new Monash Children’s hospital. He came with his father who was very interested to see the difference in care from the previous era and how far technology had improved. Mark also wanted to show staff and families with premature babies currently in the nursery that even from a rocky start in life it is possible to achieve a lot and this would have been hard to predict from his own early days.
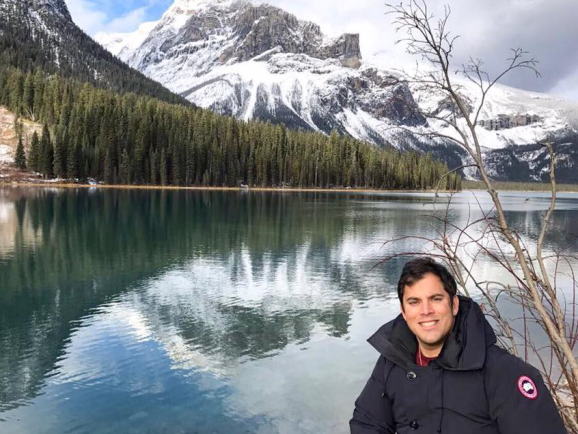
Mark spent his childhood in Australia and India and has since spent time working and studying in Dubai, England, Canada and Unites States.
Academically he excelled with a B.Sc (Econ) Hons from University of London, MBusLaw from Monash University, Australia and an MBA from the Ivy League Institute Columbia University, New York. He is also a Charted Marketer and Senior Associate of the Financial Services Institute of Australasia. He has been involved in business development, marketing and finance over many years in India, United Arab Emirates and the United States.
Socially he is a member of the Melbourne Cricket Club in Australia, Royal Western India Turf Club, Royal Bombay Yacht Club and the Royal Canadian Yacht Club and also a Board Member of the Pony Club of Australia with the aim of encouraging more people to form connections with animals through pony riding.
He has currently returned to live and work in Australia.
General News and Staff News
A big Year for Professor Lex Doyle
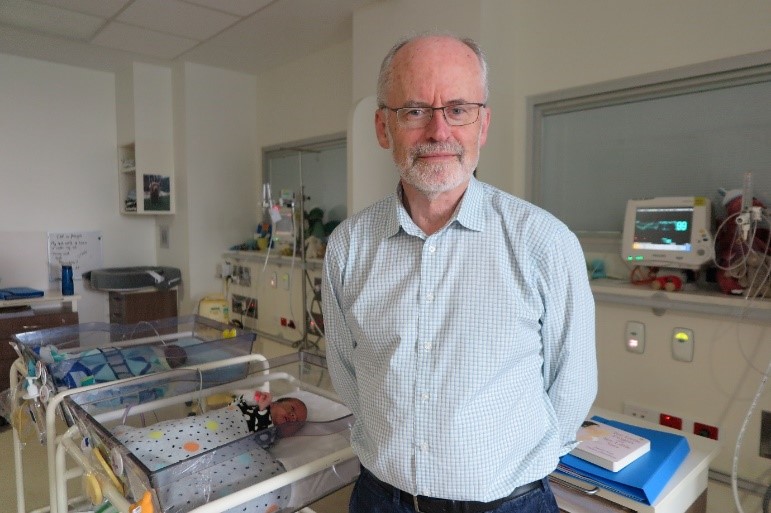
Messages of congratulations are flooding in for the Women’s Head of Clinical Research Development, Professor Lex Doyle AO after he was named an Officer of the Order of Australia in the Queen’s Birthday Honours recently.
The honour is awarded for distinguished service of a high degree to Australia or humanity at large. In Prof Doyle’s case, it recognises his distinguished service to medicine, and to medical education, as a neonatal paediatrician, academic, author and researcher.
In acknowledging the award, the Women’s CEO Dr Sue Matthews said Prof Doyle is recognised internationally as a central figure in neonatal research.
“Lex is recognised as one of the world’s leading neonatal researchers with a stellar career spanning more than 45 years.
“Receiving this award is a great achievement and I want to congratulate Lex on the outstanding contribution he has made to the Australian community and neonatal paediatrics globally.”
Prof Doyle’s career spans several decades during which he established himself as the leading expert on the long-term outcomes for premature babies, having created, with others, the Victorian Infant Collaborative Study Group in the 1980s which is continuing today; as well as working on longitudinal studies of children born at the Women’s, continuing on from the late, Bill Kitchen AM.
“It’s very humbling to receive an award that is nominated by your peers,” Prof Doyle said a recent gathering to celebrate the announcement.
“The award to me is really an award for the team, because I can’t achieve anything without the team who do all the hard work. It is really a credit to them.”
Prof Doyle began working at the Women’s in neonatal intensive care shortly after finishing his university study and placements, in the mid-1970s.
Professor Lex Doyle, the Women’s Head of Clinical Research Development, has received the prestigious Howard Williams Medal at the Royal Australasian College of Physicians (RACP) annual meeting held in Auckland this May.

Each year the medal is awarded to a clinician who is deemed to have made an outstanding contribution to improving the health of children and young people in Australia or New Zealand.
Over the course of his esteemed career, Prof Doyle has made a significant impact in the area of neonatology and paediatrics research, leading multiple studies aimed at improving outcomes for our most vulnerable infants.
Director of Neonatal Medicine, Professor Peter Davis, said Prof Doyle was an extremely deserving recipient of this prestigious award.
“Lex is universally recognised as one of the leading experts in the world on assessment of long-term outcomes after very preterm birth,” Professor Davis said. “He has led many studies which have resulted in changed practices being adopted worldwide and affecting the lives of literally thousands of infants.”
“Lex’s pioneering work and leadership in this field has not only helped to advance clinical outcomes for neonates, but has also helped to attract many trainees, masters and doctorate candidates from around the world. Lex has been very supportive of women in research, as evidenced by the number he has mentored to successful research careers,” added Associate Professor Jeanie Cheong, neonatologist and long-time research colleague and collaborator.
Over the past four decades Prof Doyle has made significant contributions to neonatology and paediatrics research; he has been published in over 550 scientific journals and has been a speaker at more than 150 conferences internationally. His expertise is sought all over the world, especially in developing countries where his work has been particularly influential.
Prof Doyle said he was humbled to receive the award, “It’s always an honour to be acknowledged by your peers but the real heroes are the families and their vulnerable babies who battle against the odds and go on to lead healthy lives, and I’m privileged to be able to play a part in making that happen,” he said.
Our Newest -Dr Amanda Kwong. Well Done Amanda
Over the past three years, Amanda Kwong has been working with the VICS 2016/2017 cohort as part of her PhD studies, specifically looking at the Baby Moves smartphone app for use with the General Movements Assessment. In November 2019, Amanda’s PhD passed successfully under supervision from Prof Alicia Spittle, A/Prof Jeanie Cheong and Prof Lex Doyle.
Amanda’s PhD explored the use of the Baby Moves smartphone app amongst infants born extremely preterm and/or extremely low birthweight. Baby Moves allows parents to record their infants’ movements at 3-4 months of age and send their videos to trained remote assessors for a General Movements Assessment, which has excellent predictive ability to detect cerebral palsy: a condition resulting in movement problems which occurs at higher rates in the extremely preterm and/or extremely low birthweight population compared with those born at term. Amanda’s PhD found that families were able to use Baby Moves successfully, but those with lower sociodemographic status tended to use the app less, regardless of their infant’s birth status. She also found that infant’s general movements change over time and that, where possible, two assessments should be completed between 12-17 weeks’ corrected age. Finally, she found that brain injury was strongly related to abnormal General Movements Assessment at 3-4 months of age, as well as motor function at 4 months’ corrected age.
Amanda hopes that her findings will generate much-needed evidence for the use of smartphone technology with the General Movements Assessment so that high-risk infants have easier access to important assessments that could diagnose conditions like cerebral palsy earlier.
2 other members of the VICS team have had academic promotions at the University of Melbourne – Alicia Spittle as Professor in the Department of Physiotherapy, and Jeanie Cheong as an Honorary Professorial Fellow with the Department of Obstetrics and Gynaecology

An important area of Alicia’s hard work, applicable to the VICS group was with developing the baby moves app with Amanda Kwong.- The Baby Moves smartphone app amongst infants born extremely preterm and/or extremely low birthweight. Baby Moves allows parents to record their infants’ movements at 3-4 months of age and send their videos to trained remote assessors for a General Movements Assessment, which has excellent predictive ability to detect cerebral palsy: a condition resulting in movement problems which occurs at higher rates in the extremely preterm and/or extremely low birthweight population compared with those born at term.

Prof Jeanie Cheong is a Neonatal Peadiatrician with expertise in neonatal neurology, neuroimaging and long term follow up. She is based at the Royal Women’s Hospital and is the lead clinician in the Growth and Development clinic.
Jeanie has several affiliations; as the medical/neurological Team Leader of the Victorian Infant Brain studies group within Murdoch Children’s, the Convenor of the Victorian Infant Collaborative Study group, and Associate Professor with the Department of Obstetrics & Gynaecology at the University of Melbourne. She is the lead investigator on a National Health and Medical Research Council funded study looking at long term neurodevelopmental outcomes and brain structural changes following late preterm birth.
We congratulate all of these staff members on their outstanding achievements.
The Royal Women’s Hospital celebrates World Prematurity Day
On November 17, 2019, we celebrated World Prematurity Day, a day to acknowledge the millions of families affected by prematurity worldwide, to reflect on the many great achievements in neonatal care, and to remember all babies born preterm.
In recognition of this important day, The Royal Women’s Hospital invited families, clinicians and researchers to a free public seminar on 18 November.
The opening address was given by Shussanah Morris, Co-Founder and CEO of the Life’s Little Treasures Foundation, who shared her story of her daughter, Molly Rose’s birth and time in NICU. We were delighted to have Molly Rose and her dad attend the seminar.

This was followed by presentations from three clinician-researchers whose work focusses on improving outcomes of babies born preterm.
Dr Penny Sheenan spoke about the role of a Preterm Labour Clinic in screening for, and prevention of preterm birth.
Dr Rose Boland provided an overview of the role of the statewide neonatal emergency transport service (NETS/PIPER) in transporting premature and sick babies to a NICU.
Associate Professor Jeanie Cheong discussed long-term outcomes of children born very preterm in Victoria, including important health outcomes into young adulthood.
There was an opportunity for parents and family members to ask questions from the presenters before the evening concluded.
We are aiming to host this
seminar as an annual event at the Royal Women’s Hospital.
To update us with your current contact details, including your email address OR
To find out more about the Victorian Infant Collaborative Study, visit our website: